Leonard Pinkney knew for years that his DNA was against him — he has family history on both sides of diabetes, blood pressure and heart attacks.
The Susquehanna Twp. man was diagnosed with diabetes 24 years ago, had a quadruple bypass 14 years ago and has been on blood pressure medicine since 1975.
A year and a half ago, Pinkney’s kidneys began to fail and he was diagnosed with end stage renal disease. Dialysis was his only option, short of a kidney transplant.
Though many people know that failing kidneys require dialysis, few may know that there are different types of dialysis from which to choose.
Pinkney goes to a dialysis unit three times a week for four hours and watches TV while his blood gets cleaned. He has to plan his life around these visits, but he’s not complaining.
“It’s either this or I die,” said Pinkney, 76, who is a retired equal opportunity manager from the U.S. Department of Defense. “I’ve dedicated my life to getting these treatments so I arrange everything else around them. I am a positive person, and I know this is the best I can do.”
Pinkney has the option of doing his dialysis at home, but he chooses to go to a unit because he says he’s not comfortable with taking on the medical responsibility of doing it himself. He’s also investigating whether he is a candidate for a kidney transplant.
Meanwhile, as long as he “follows the rules,” he said he feels good, can still play golf and can still travel with his wife, Sherlene. He makes sure he schedules his trips near a dialysis unit.
An often silent disease
The kidneys’ main function is to clear the blood of toxins and excess fluid through urine. Kidneys also make the most potent form of vitamin D in the body and are important to bone health.
Dialysis, a treatment that does some of what the kidneys naturally should do themselves, is needed when the kidneys cannot get rid of the toxins and/or excess fluids that build up in the bloodstream, said Dr. Julie Rothman, a nephrologist with Nephrology Associates of Central PA in Camp Hill.
Besides transplant, dialysis is the only option when end stage renal disease occurs, which happens when about 85 percent to 90 percent of kidney function is lost, she said.
About half a million people in the United States are on dialysis because of end stage renal disease, a very intrusive disease because of its constant effects on daily life in terms of what patients can eat and drink, time-consuming dialysis treatments and the need for a number of medications.
However, unlike cancer, end stage renal disease fails to get people’s attention — or attempts at prevention — even though it is a great burden on the patient and society to treat it, Rothman said.
“Unfortunately, kidney disease is often silent until end stage renal failure occurs, which can lead to uremic poisoning,” she said. Signs of this include sleepiness, nausea, vomiting, nightmares, tremors, shortness of breath and swelling. It can also lead to inflammation around the heart.
“The No. 1 cause of end stage renal disease in this country is diabetes and we have an epidemic of that,” Rothman said. “Adults over age 40 and people with diabetes or high blood pressure need to be screened annually for kidney disease.”
Older men who have an enlarged prostate or prostate cancer and people with kidney stones can also be at risk for developing kidney disease, she said. There are many other reasons for kidney disease, but these are the most common. There are also many types of inflammatory kidney diseases that can cause end stage renal disease.
Choosing dialysis
Treating the disease involves dialysis, and there are two main types: hemodialysis, of which there are a few varieties, and peritoneal dialysis.
“How do you know which is right for you? The doctor and the patient discuss it; the doctor suggests what he or she thinks, but ultimately it’s up to you unless there’s a reason why you’re not a candidate for one or the other type,” Rothman said.
Hemodialysis involves using an artificial kidney called a dialyzer to remove waste and extra fluid from the blood. This is the type of dialysis that Pinkney chose.
To get access to the blood, surgeons have a few options, Rothman said. They can join an artery to a vein (usually in an arm) in a number of different ways for permanent access to the blood. Otherwise, a temporary, large IV called a catheter can be put in a vein in the neck. This is usually done only in an emergency situation or if no other access is possible.
With peritoneal dialysis, the blood is cleaned inside the body. A plastic catheter surgically implanted into the abdomen allows access so that a “bath” of dialysate can be slowly put into the belly to flush out the toxins and waste products, Rothman explained. Tiny blood vessels in the belly can act like an artificial dialyzer.
There are two main ways to do peritoneal dialysis. With continuous ambulatory peritoneal dialysis, the patient puts a bag of dialysate into the belly through the catheter four to five times daily. The patient goes about their day while the dialysate stays inside for four or five hours, drawing out the toxins and excess fluid, before draining back into the bag and getting thrown away.
Continuous cycler peritoneal dialysis usually is done at home using a cycler, a machine that puts fluid in and drains it multiple times during the night while you sleep.
“If there is no bowel disease or other contraindication for this, it’s an excellent way to go because you do it yourself at home. You also have the freedom not to sit in a dialysis unit four hours, three times a week,” Rothman said.
Patients must learn to be very sterile with the process, however, or peritonitis — inflammation of the peritoneum — can occur, she said. This causes fever and extreme pain and requires antibiotic treatment.
If hemodialysis is chosen, it can be done during the day in a dialysis unit or at home five to six times a week for a shorter period of time that can be planned out around a patient’s life schedule, Rothman said.
Patients who go to a unit for dialysis can watch TV, listen to the radio, read or even nap through their treatments, said Tammy Loper, nurse manager at Liberty Dialysis in Lemoyne.
“It becomes like their own little community where they learn to care about each other and support each other,” she said.
How people view the intrusion of dialysis into their lives depends on their age and other medical conditions they have, Loper said. “Some people get angry at first, but most come to realize that without it, they wouldn’t be here, so they end up thankful for it,” she said.
There’s also the option for nocturnal hemodialysis, where patients sleep at the dialysis center three times a week and get an eight-hour treatment. Because the nocturnal dialysis takes toxins and fluids out over a longer period of time, patients are much less likely to experience common side effects of dialysis such as low blood pressure and cramping.
“It’s like shoes; there are different fits for every patient,” Rothman said.
Avoid dialysis – Screen your kidney function
Often kidney disease is silent until it is advanced and dialysis is needed. That makes it especially important that people at increased risk for chronic kidney disease have regular screening tests for protein in the urine, a blood test for blood creatine and blood pressure measurement.
You may have an increased risk for kidney disease if you:
Are older
Have diabetes
Have high blood pressure
Have a family member with chronic kidney disease
Are an African-American, Hispanic American, Asian and Pacific Islander or American Indian
Source: National Kidney Foundation
Camp Hill nephrologist Dr. Julie Rothman uses vowels as a way to help people understand when they may need dialysis if medications have failed or won’t suffice:
A: Acidemia – This occurs when acids build up in the body as a result of non-functioning kidneys.
E: Electrolyte imbalance – The kidneys regulate the body’s salts and potassium, which can become unbalanced due to kidney disease.
I: Intoxication – Dialysis may be able to rid the body of either accidental or intentional drug overdose.
O: Overload of fluids – Edema, swelling due to fluid retention or congestive heart failure can result due to the kidneys not working properly.
U: Uremia – When signs and symptoms of uremic poisoning are present (nausea, nightmares, swelling, shortness of breath, tremors, poor appetite), dialysis is needed. ~pennlive.com~
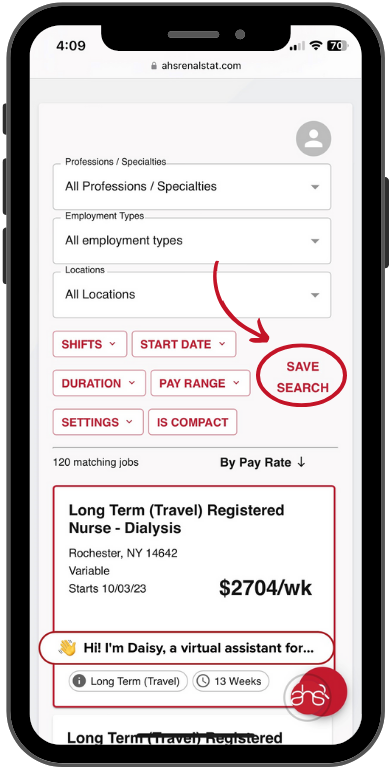
AHS RenalStat is one of the fastest growing dialysis staffing firms in the United States. We have more than 27 years of renal staffing experience under our belts. Dialysis staffing is our business—it’s what we enjoy, understand, and do every day. We are experts in providing you with the most qualified dialysis nurses and certified dialysis technicians available. What sets us apart from others is that we are truly a full service dialysis staffing firm. We provide all three types of placement: permanent placement, travel nurses and technicians, and relief (per diem) candidates. No one else in the industry provides this, and it sets us apart!
For more information on dialysis staffing, contact:
AHS RenalStat
A Leader In Dialysis Staffing
877-309-3546
www.ahsrenalstat.com