As a dialysis patient, summer can sometimes be challenging. The heat and loss of fluids can take a toll on your body.
Research shows a healthy body needs up to eight glasses of water a day to maintain fluid balance. For people with end stage renal disease (ESRD), these normal amounts of fluid may cause problems. Too much fluid can build up in the body and be dangerous.
Fluid control for those on hemodialysis:
The goal of fluid restriction is to help you feel comfortable before, during and after your dialysis sessions. Even though dialysis gets rid of excess fluid and waste in the body, it is not as effective as healthy kidneys. Why? Healthy kidneys work all the time—24 hours a day, 7 days a week. Most people on hemodialysis get treatments three times a week for about three or more hours at a time. This means, in the days between your dialysis treatments, your body holds on to excess fluid and waste your kidneys cannot remove.
Going over your recommended fluid allowance can lead to too much fluid building up in your body between treatments. This build up causes swelling and increases your blood pressure, which makes your heart work harder. Too much fluid can build up in the lungs, making it difficult for you to breathe.
Hemodialysis removes fluid as the blood is filtered through the dialysis machine. However, there is a limit on how much fluid can be safely removed during a dialysis session. If you exceed your fluid allowance, more fluid must be removed. Your body may not be used to having so much fluid removed at once. Some people experience muscle cramping during dialysis when they gain too much fluid weight. Taking out a lot of fluid can also cause a drop in blood pressure, which can leave you feeling nauseated, dizzy and weak after the treatment. Sometimes, an extra dialysis session may be required to remove all the extra fluid.
Fluid control for those on peritoneal dialysis:
People on peritoneal dialysis (PD) may not be as limited with their fluids as people on hemodialysis. This is because PD treatments are performed every day, unlike hemodialysis, which is done several times a week.
Although patients on PD are allowed more liquid, they are encouraged to keep track of their fluid intake and the amount of fluid removed in their dialysis exchanges. Too much fluid can still lead to complications like swelling, high blood pressure and shortness of breath.
How is fluid restriction determined?
Fluid restriction may vary for each individual patient. Factors such as weight gain between treatments, urine output and swelling are considered. If you are on hemodialysis, your weight is recorded before and after your dialysis session. Your nurse uses weight changes to help determine how much fluid to remove during dialysis. If you are on peritoneal dialysis, your nurse will have you record your weight every day. Sudden weight gain may mean you are drinking too much fluid. Your dietitian will coach you on individual goals for your fluid intake.
What are the complications associated with too much fluid?
For dialysis patients, the complications of excess fluid are:
High blood pressure
A sudden drop to low blood pressure (generally occurs during hemodialysis)
Shortness of breath (and in some instances, fluid in the lungs)
Heart problems, which can include a fast pulse, weakened heart muscles and an enlarged heart
Exercise and fluid intake:
Before you start an exercise program, let your doctor and health care team know. Exercise may change your fluid requirements, especially if you are exercising and perspiring heavily. Your dietitian can coach you on how much fluid to drink. Talk to your dietitian before making changes in your fluid intake.
Tips for managing your thirst during the heat of the summer:
Your dietitian—as well as fellow patients—can give you many helpful hints to manage your thirst. Here are some tips to get you started:
Salty and spicy foods make you thirsty. To help control thirst, your dietitian will recommend that you limit the amount of sodium and spicy foods in your diet.
Be aware of hidden fluids in foods. Your dietitian will provide you with guidelines to help you count your fluid intake. Fluid isn’t just what you drink; it’s also in what you eat. Your dietitian will suggest limiting foods with high water content, such as: gelatin, watermelon, soup, gravy and frozen treats like PopsiclesTM and ice cream.
Stay cool. Keeping cool will help reduce your thirst, especially in warmer weather. Try drinking cold liquids instead of hot beverages. And, if you’re thirsty between meals, try snacking on approved vegetables and fruits that are ice cold.
Sip your beverages. Sipping will let you savor the liquid longer. Use small cups or glasses for your beverages.
Try ice. Many patients find that ice is more satisfying than liquids. Try freezing your allotted amount of water into an ice tray. You can also try freezing approved fruit juices in ice trays for a special treat. Remember to include the ice you consume when tracking your fluid intake.
Take your medicines with your meal, if possible. Try swallowing pills with applesauce instead of liquids. (Check with your doctor before changing the times you take medications.)
Battle dry mouth. Dry mouth can be uncomfortable. Instead of drinking fluid to refresh your mouth, try using mouthwash or brushing your teeth. Sucking on hard candy or a wedge of lemon or lime will also help.
If you have diabetes, maintain good blood glucose levels. High blood glucose levels will increase your thirst. Managing your diabetes by following your doctor and dietitian’s recommendations will help you manage your thirst.
Restricting fluids isn’t easy, but if you get tips from your dietitian and ask other patients what they do, you may find it isn’t as difficult as you thought. The reward is you will feel better by preventing uncomfortable treatments, cramping and blood pressure fluctuations and stay healthier.
source: davita.com
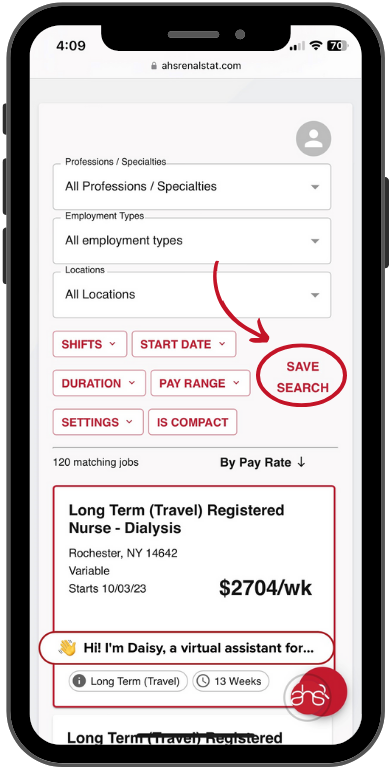
AHS RenalStat
A Leading Dialysis Staffing Agency
[email protected]
877-309-3546
www.ahsrenalstat.com
QUICK APPLY